Breech Delivery Vaginal Breech (378)
| Please report any inaccuracies or issues with this guideline using our online form |
The incidence of breech presentation is 25% at 28 weeks, 16% at 32 weeks and 3-4% at term. The authors of the term breech trial recommended “the best method of delivering a complete or frank breech singleton at term is by planned lower segment caesarean section”. Nevertheless there are women with a breech presentation at term who will make an informed choice to have a trial of vaginal breech delivery. There is no good evidence to support that caesarean section is the safest mode of delivery for the preterm breech. There are also women who will present in advanced labour with an undiagnosed breech presentation, for whom caesarean section may not be an option.
IT IS THERFORE IMPORTANT THAT CLINICIANS ARE FAMILIAR WITH TECHNIQUES FOR ACHIEVING SUCCESSFUL VAGINAL BREECH DELIVERY
The same manipulations are employed when delivering a breech or a Caesarean section. Master them when doing CS for Breech presentations.
Management of Vaginal Breech Delivery: In women who decline or are unsuitable for Caesarean section Types of Breech
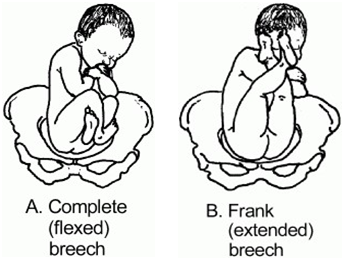
There are four types of breech presentation. They are determined by the way in which the fetal legs are flexed or extended, and these have implications for the birth
- Complete or Flexed Breech: The flexed breech occurs more commonly in the multigravid woman. Flexed breech is when the fetus sits with the thighs and knees flexed with the feet close to the buttocks. (see Diagram A)
- Frank or Extended Breech: This is the commonest type of breech presentation and occurs most frequently in the primigravid woman towards term: the fetal thighs are flexed, but the legs are extended at the knees and lie alongside the trunk, the feet being near the fetal head. (see Diagram B)
- Footling presentation: This type of breech is more likely to occur when the fetus is preterm, but is relatively rare. Footling breech is when one or both feet present below the fetal buttocks, with hips and knees extended. There is increased risk of cord prolapse.
- Knee presentation: This is the least common. This occurs when one or both knees present below the fetal buttocks, with one or both hips extended and the knees flexed.
Management of First Stage of labour
On admission
- Confirm breech presentation.
- Clinical assessment of the fetal size
- Assess whether pelvis seems to be adequate.
- Ultrasound by a competent practitioner is useful to:
- assess the type of breech
- Locate the placenta,
- Assess size of the fetus (unless AC performed within last 14 days)
- Determine the attitude of the fetal head.
- Fetal heart activity
- Amniotic fluid volume
- Whether neck is extended or not
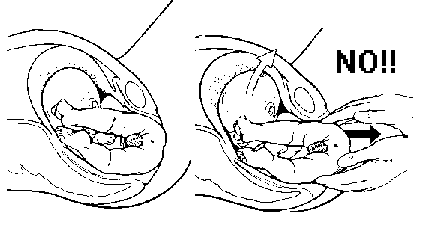
N.B There should be no hyperextension of the fetal head. If present: explain to woman what this means. This is a contra-indication to attempting vaginal birth.
Following above assessment:
- Discuss management options and confirm that the mother still wishes to have a vaginal breech delivery.
- Obtain written consent including options of emergency interventions (Breech extraction and CS)
- Inform the consultant obstetrician on call
- Inform on-call anaesthetist / paediatric staff
- Obtain IV access: 14g cannula
- Offer epidural anaesthesia (not essential but helpful)
- If membranes rupture spontaneously, vaginal examination is required to exclude umbilical cord prolapse.
- If membranes are still intact then amniotomy should only be performed for usual indications.
- Continuous fetal monitoring should be used.
- Fetal blood sampling can be performed from the fetal buttocks. The indications, technique and interpretation used should be the same as for cephalic presentations.
- Oxytocin may be used with caution; after discussion with senior obstetrician; usual regime depending on parity.
Management of Second Stage:
Ideally a consultant obstetrician with experience of vaginal breech delivery should be present for the management of the second stage if time allows.
Basic principles:
- A scrubbed assistant should be present if possible
- Avoid handling the breech as it descends until leg manipulation required
- Ensure good maternal effort
- Do not touch the cord
- Keep the sacrum anterior
- Empty bladder
- Begin active pushing when breech has descended to the pelvic floor.
- Delay Lithotomy position until anus is visible over the fourchette.
- Consider episiotomy at this time.
- Allow spontaneous rotation to sacrum anterior position.
- If legs extended, deliver legs by applying pressure in the popliteal fossa to flex the legs at the knee joint.
- As the trunk descends with maternal effort, the tip of the scapula of the anterior shoulder becomes visible. The anterior arm should be delivered by splinting the humerus between 2 fingers. The other shoulder should rotate spontaneously to allow similar delivery of the other arm.
- If the arms are extended or a nuchal arm is diagnosed Lovsett’s manoeuvre should be used Apply gentle traction using a femero-pelvic grip and deliver one arm by clockwise rotation to the oblique, followed by counter clockwise rotation to the oblique to deliver the other arm.
N.B Lovsett is not a routine part of a vaginal breech delivery

- Support the baby as the head engages.
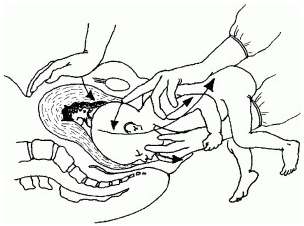
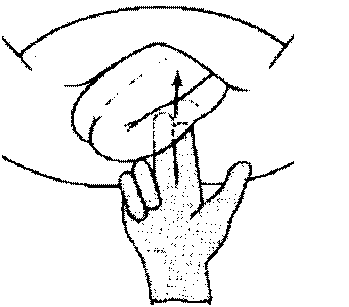
- Use Mauriceau-Smellie-Veit (MSV) manoeuvre to complete delivery. The MSV manoeuvre encourages flexion of the fetal head. Place one hand above the fetus with one finger on the fetal occiput and one finger on each of the fetal shoulders. The other hand should be placed below the fetus and 2 fingers should be placed on the maxillae (not in the mouth). Some practitioners use their 2nd and 4th fingers for this and place their middle finger under the chin for triangular stability. The fetal body is raised upward in an arc completing delivery
Application of Forceps to After Coming Head
In up to 20% of cases forceps may be required to deliver the fetal head.
This is not as difficult as it might appear. Practise on a manikin is advised to become familiar with the technique.
- Do not panic
- The head is generally direct OA or no more than 15° left or right.
- Assistant should gently lift and support the baby without undue traction. Its body can be wrapped in a towel to keep it warm
- Select Mid Cavity forceps, such as Simpsons. Do Not use Wrigley’s.
- Apply Forceps using a standard approach. Once the first blade is applied any lateral deviation can usually be corrected to DOA.
- Once the forceps are applied, check application and lock as next contraction commences
- Gentle downward traction
- Start upward traction once chin on perineum (evaluate for episiotomy if not already done; usual care and angulation)
- Controlled and slow delivery of head
- Transfer baby to waiting paediatric team
- Take a cord PH
- Deliver placenta and repair perineum
- Record Comprehensive note