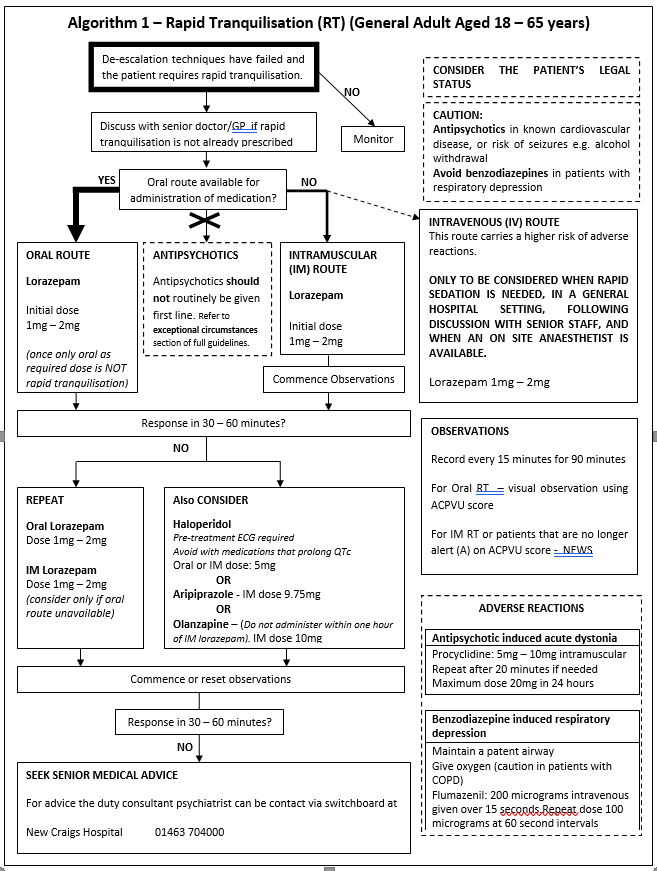
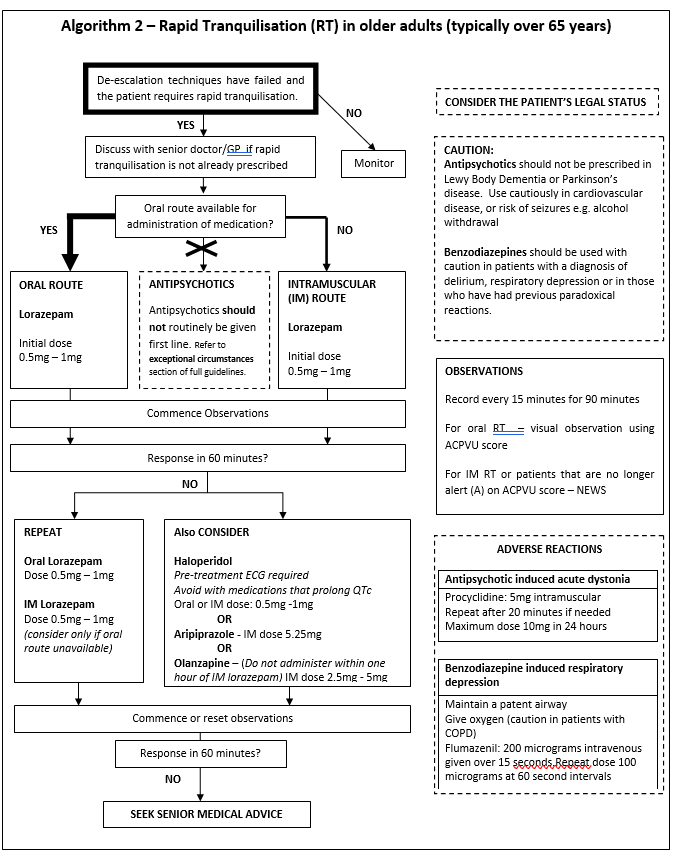
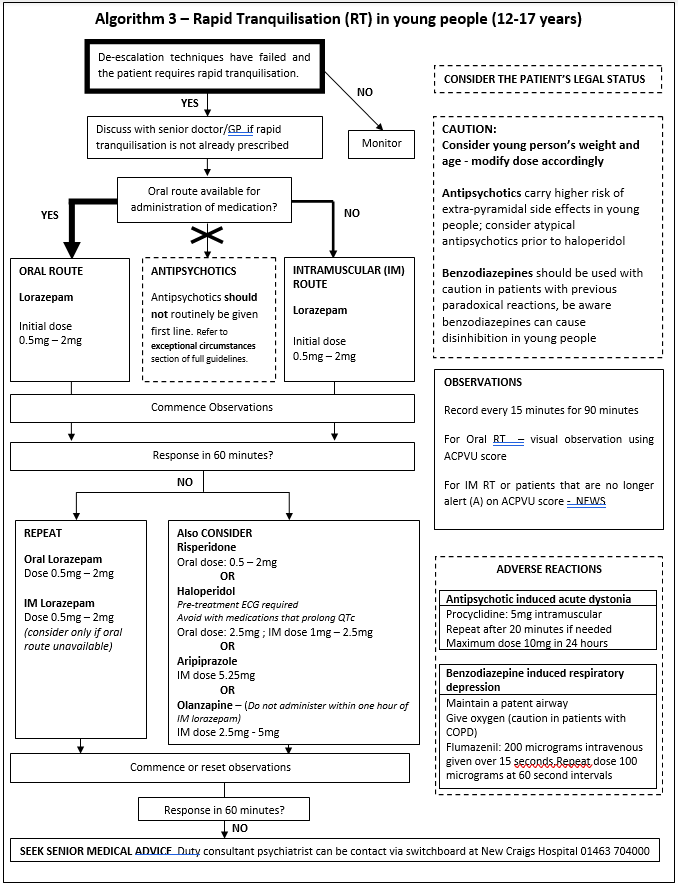
These quick reference algorithms are summaries for use in clinical settings and are to be used alongside the full guideline.
The goal of rapid tranquillisation is “to achieve a state of calmness without sedation, sleep or unconsciousness, thereby reducing the risk to self and/or others while maintaining the ability of the patient to respond to communication”(NICE, 2005) when appropriate psychological and behavioural approaches have failed to de-escalate acutely disturbed behaviour.
A single as required dose of oral medication is not rapid tranquilisation.
Patient safety
The safety of the patient and others is the primary focus of this guideline. There are various considerations:
- Non Pharmacological Approaches – can these methods be used to improve the situation?
- Cumulative Antipsychotic Dose – Take into account regular prescriptions. If not it is possible to exceed maximum daily dose of antipsychotics placing the patient at increased risk of adverse events
- Combinations – the use of two or more antipsychotics should be avoided where possible due to the risk of additive side effects including QT prolongation. This is a particularly important consideration in rapid tranquilisation where the patient’s physical state predisposes to cardiac arrhythmia.
- Age Specific Doses – there are important differences in the medication and doses in older adults and young people compared to in adults aged 18-65. This is covered in the age-specific algorithms.
- Co-morbid neurological disorders – be aware of the risk of antipsychotics, especially in Parkinsons Disease and Lewy Body dementia where these medications should be avoided, and in epilepsy where the seizure threshold is reduced.
Key guideline updates
- A benzodiazepine (lorazepam) is the first line drug of choice to achieve rapid tranquilisation.
- Antipsychotic medication is considered a second line medication, but can be considered first line in exceptional circumstances.
The use of haloperidol has the following important updates:
- Haloperidol can prolong the QTc and is contraindicated with other such medications (see Appendix 1 for a list of common medications that can prolong the QTc).
- The use of haloperidol in such a combination renders treatment unlicensed and should be avoided where possible. If clinical circumstances make the use of such combinations unavoidable and all other options have been considered ensure the rationale for treatment is clearly documented. Consider increased monitoring of ECG and biochemical parameters.
- The SPC for haloperidol requires a pre-treatment ECG. If circumstances make this impractical avoid haloperidol, or if use is unavoidable a clear justification must be documented.
- The maximum cumulative dose of haloperidol over 24 hours (oral and/or IM) in adults aged 18 years and above is now 20mg. The maximum cumulative dose in elderly patients is 5mg over 24 hours.
Please refer to the full policy (Section 9) if there is uncertainty about the legal status of the patient and the use of rapid tranquilisation.
The following three algorithms outline rapid tranquilisation options in the different patient age groups.