- Chlamydia trachomatis - 40% of cases of NGU
- Mycoplasma genitalium – > 20% of symptomatic urethritis
- Ureaplasma urealyticum – role unclear. Biovar 2 may account for 5-10% NSU
- Trichomonas vaginalis
- Herpes simplex virus
- Adenovirus
- Others: Epstein Barr Virus, N.Meningitidis, Haemophilus sp, Candida sp, foreign bodies, urethral stricture, non infective (idiopathic/possibly inflammatory)
Urethral discharge in men

Urethritis = inflammation of the urethra indicated by the presence of polymorphonuclear leucocytes (PMNLs).
Gonococcal urethritis = when N.gonorrhoea is detected.
Non-gonococcal urethritis (NGU) = when no N.gonorrhoea is detected.
Non-specific urethritis (NSU) = non-gonococcal, non-chlamydial urethritis.
Symptoms
- Urethral discharge
- Dysuria
- Urethral irritation
- Fever, painful lymph nodes and / or haematuria if HSV causative agent
- Nil
Signs
- Urethral discharge
- Tender inguinal lymphadenopathy if HSV causative agent
- Nil
Complications (occurring in <1%)
Epididymo-orchitis
Sexually acquired reactive arthritis (SARA)
Confirmed by demonstration of PMNLs in the anterior urethra.
1. Gram stained urethral smear
Technique: insert a plastic inoculation loop at least 1 cm into urethra and withdraw, gently scraping the walls of the urethra, spread thinly on a dry slide for microscopy.
Definition: 5 or more PMNL per high-powered field averaged over 5 fields.
Ideally the slide should be made >2 hours since last passing urine. In symptomatic patients who have recently voided/who have normal microscopy consider early morning smear (EMS) – arrange to return first thing having held urine overnight.
2. Gram stained “threads” from a first pass urine (FPU)
sample if no material gained from urethral smear and threads visible.
>10 PMNL per HPF in at least 5 fields.
|
Further Investigations
- First pass urine (FPU) for CT/GC NAAT.
- We do not do routine testing for M. Genitalium at present but this can be considered in cases of persistent urethritis (discuss with senior GUM cover).
- GC cultures if diagnosis suggestive of possible GC urethritis (profuse purulent discharge, microscopy with paired cocci suggestive of possible NG, contact of GC). The general rule is to
do cultures if treatment for gonorrhoea is considered – see Gonorrhoea protocol for correct plating technique.
Additional investigations to consider:
- If symptoms suggestive of UTI send mid stream urine (MSU).
- If symptoms suggestive of HSV infection consider urethral swab sent in red-topped universal transport medium (UTM) for HSV PCR.
Patients seen at local clinics with symptoms or signs suggestive of urethritis should be referred to Galashiels for microscopy (and GC culture if needed). When patients decline or are unable to attend, the diagnosis can be made on the following basis:
- Presence of mucopurulent discharge on examination.
- Urinalysis of FPU: Leucocytes + or more.
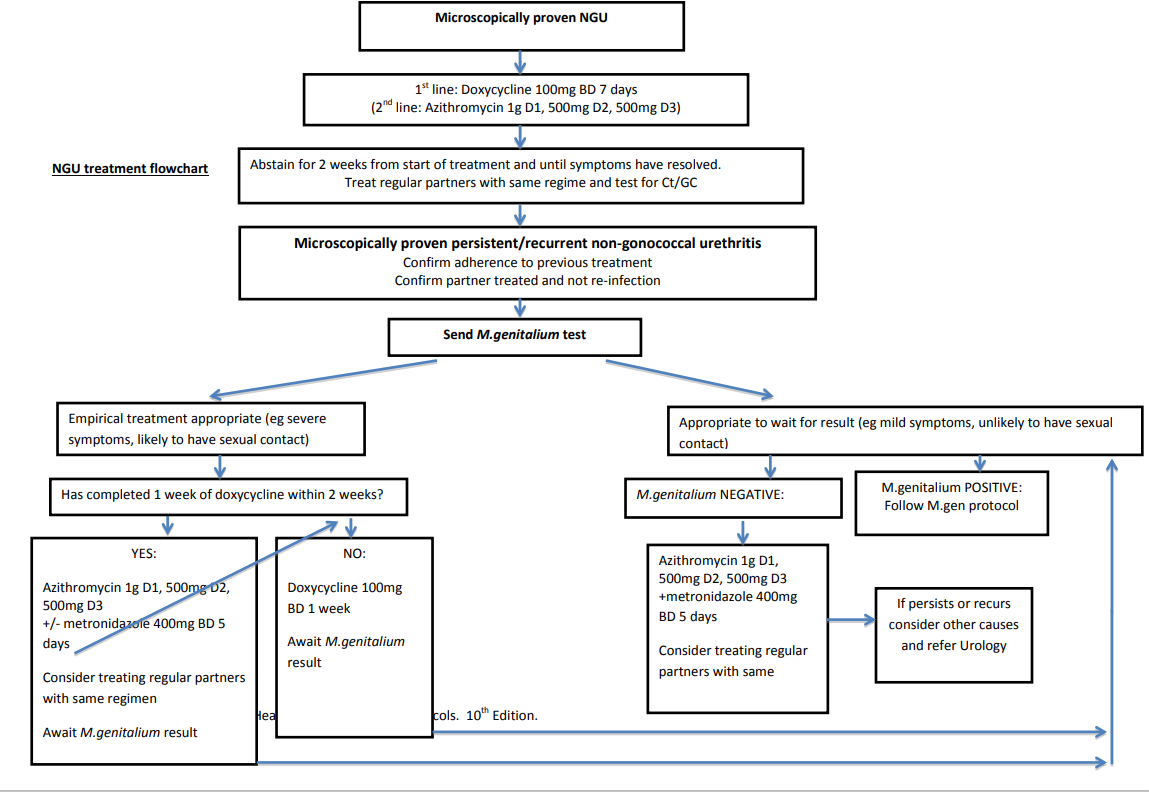
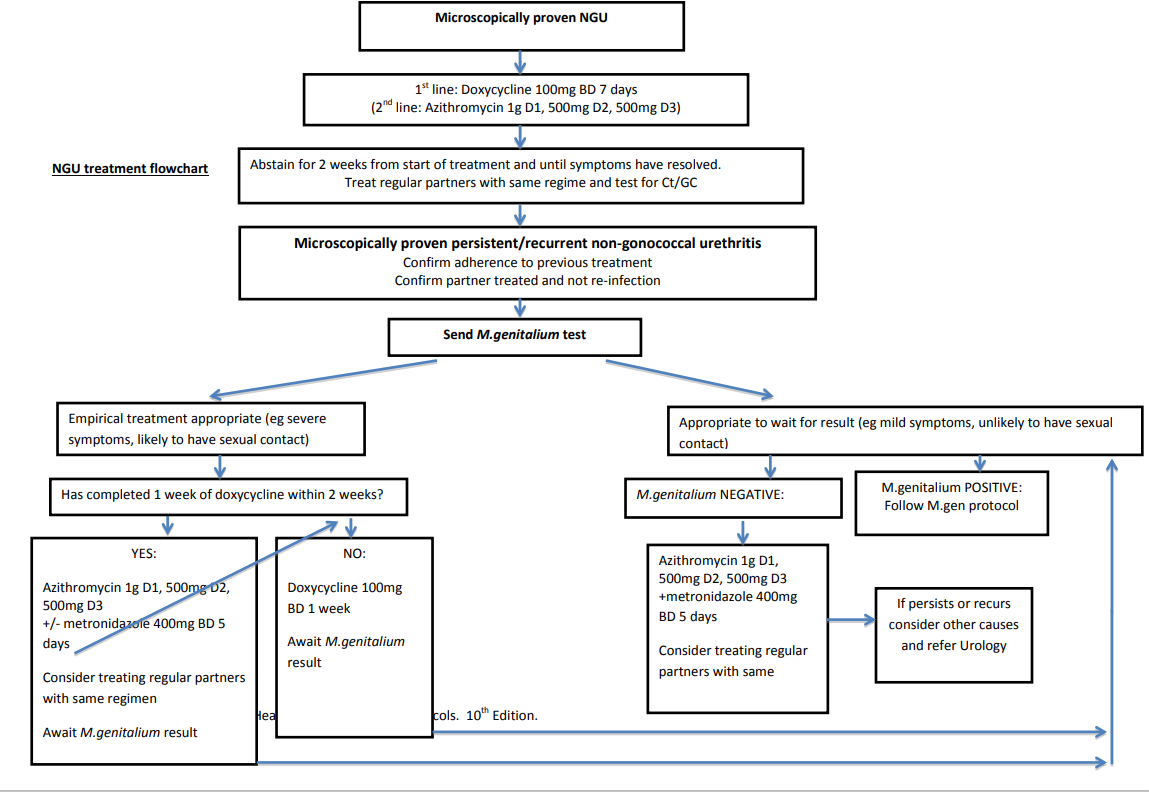
Management – see NGU treatment flowchart.
Non-gonococcal urethritis
Doxycycline 100 mg orally twice a day for 7 days Alternative:
|
Gonococcal urethritis
See GUM protocol Section 2 for management and PN.
Non-gonococcal urethritis: additional management points
Sexual contacts
- Partner notification should be discussed with all patients.
- All partners in the preceding 4 weeks should ideally be treated empirically (with same regime as index patient – unless recurrent/persistent NGU and suspected M.genitalium) and advised to attend for STI screening.
Patient information
- An explanation of the cases of urethritis including non-infective causes.
- Explanation of potential short- and long-term complications.
- Avoidance of sexual contact until both partners treated and for 2 weeks after the start of antibiotics - this is likely to reduce the risk of selecting/inducing macrolide resistance if exposed to M.genitalium or Neisseria gonorrhoeae which would make these infections more difficult to treat.
- Provide link to written information – patient info leaflet.
Follow up
No follow up is necessary.
Persistent/recurrent NGU
- Persistent NGU – when symptoms do not resolve following treatment and ongoing urethritis is confirmed microscopically. There is no specific guidance on the point at which symptoms are regarded as persistent. Patients should be asymptomatic at 2 weeks after start of treatment, although mild symptoms may continue for longer and are commonly experienced in the absence of any persisting microscopic evidence of NGU.
- Recurrent NGU - recurrent symptomatic microscopically confirmed urethritis occurring up to 90 days following treatment of acute NGU.
- Only diagnosed in the presence of >4 PMNL per HPF (min 5 fields) on gram stained urethral smear.
- Remember:
- Confirm adherence to previous treatment
- Confirm any regular partners have been treated
- Exclude re-infection
If diagnosis confirmed microscopically
Send sample for Mycoplasma genitalium - refer to Mycoplasma Genitalium Protocol – GUM protocol Section 21.
Management of confirmed persistent/recurrent NGU - see NGU treatment flowchart
If empirical treatment appropriate – eg severe symptoms, likely to have sexual contact
- If patient has completed 1 week of doxycycline within last 2 weeks:
Azithromycin 1g D1/500mg D2/500mg D3
+/- Metronidazole 400mg BD for 5 days
Consider treating regular partners with same antibiotics
Await M.genitalium result - If patient has not completed 1 week of doxycycline within 2 weeks:
Doxycycline 100mg BD for 7 days
Await M.genitalium result
If appropriate to wait for M.genitalium result – eg. mild symptoms, unlikely to have sexual contact
If M.genitalium Positive – follow M.genitalium protocol
If M.genitalium negative
Treat with azithromycin 1g D1/500mg D2/500mgD3
PLUS metronidazole 400mg BD for 5 days.
Ongoing symptoms but non-diagnostic urethral smear
Some patients complain of ongoing symptoms but urethral smear is not indicative of ongoing infection. In these cases:
- Ensure MSU sent and negative
- Firm reassurance that no evidence of infection or inflammation
- Discourage repeated self-examination
- Consider chronic pelvic pain
- Consider Urology referral.